CERVICAL TUMORS( 04 -06 Old batch students)
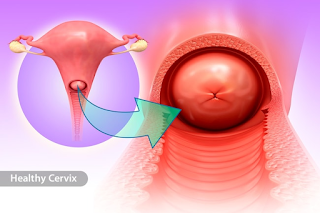
About the cervix
Cervical cancer starts in the cervix, which is the lower, narrow part of the uterus. The uterus holds the growing fetus during pregnancy. The cervix connects the lower part of the uterus to the vagina and, with the vagina, forms the birth canal.
About cervical cancer
Cervical cancer can grow from the surface of the cervix seen in the vagina, called the ectocervix, or from the canal going from the vagina to the uterus, called the endocervix. There are 2 main types of cervical cancer named for the type of cell where the cancer started. Other types of cervical cancer are rare.
Squamous cell carcinoma makes up about 80% to 90% of all cervical cancers. These cancers start in the cells on the outer surface covering of the cervix.
Adenocarcinoma makes up 10% to 20% of all cervical cancers. These cancers start in the glandular cells that line the lower birth canal in the internal portion of the cervix.
The squamous and glandular cells meet at the opening of the cervix at the squamocolumnar junction, which is the location at which most cervical cancers.
- Squamous lesions:
- Invasive squamous lesions are now classified in 2 main categories: HPV associated and HPV independent
- HPV independent squamous cell carcinomas are rare but their existence is now acknowledged as they may behave more aggressively than the more common HPV associated lesions
- Glandular lesions:
- Both preinvasive and invasive glandular lesions are now classified in 2 main categories: HPV associated and HPV independent
- HPV associated adenocarcinomas can be classified using terminology from previous classification; however, they need to be distinguished, as a group, from HPV independent tumors
- HPV independent adenocarcinomas are most frequently of the gastric type (with both in situ and invasive forms)
- Other distinct types include clear cell and mesonephric carcinomas
ETIOPATHOGENESIS OF CERVICAL CARCINOMA
Human Papilloma virus is currently considered to be the most important agent in cervical oncogenesis.
50% of virus after infection is cleared with in 8 months and 90% with in 2 years
Clearance depends upon HPV type and immune status
Increased persistence of virus is associated with risk of developing malignancy
Risk factors for cervical neoplasia
– Early age at first intercourse
– Multiple sexual partners
– Increased parity
– A male partners with multiple previous sexual partners
– The presence of cancer associated HPV
– Certain HLA & viral subtypes
– Exposure to oral contraceptives & nicotine.
HPV cannot infect mature squamous epithelium covering ectocervix, vaginal mucosa and vulva
Establishment of HPV infection requires damage to the surface epithelium, which allows the virus access to the immature cells in the basal layer epithelium.
Immature metaplastic squamous epithelium is also vulnerable to HPV infection.
Although HPV infects immature squamous cells, viral replication occurs in maturing squamous cells
Ability of HPV to act as carcinogen depends upon the viral protein E6 and E7 which interferes with the activity of tumor suppressor proteins that regulate cell growth and survival
Viral E7 protein
binds the hypophosphorylated (active) form of RB and promotes its degradation via the proteasome pathway
binds and inhibits p21 and p27, two important cyclin dependent kinase inhibitors
Removal of these controls not only enhances cell cycle progression, but also impairs the ability of cells to repair DNA damage.
Viral E6 protein
Binds to tumor suppressor protein p53 and promote its degradation by the proteosome
This causes defect in DNA repair
It upregulates the expression of telomerase which leads to cellular immortalization
Viral protein E5 is responsible for koilocytic change i,e. perinuclear halo
Types of HPV
Low risk HPV (6,11, 42, 44) – These viruses leads to lesions like Warts and condyloma accuminata. they rarely lead to invasive carcinoma
High risk HPV (16, 18, 31 33, 35) – These viruses leads to carcinomas
The physical state of virus differs in different lesions
In cancers viral DNA is integrated with host DNA. This configuration increases the expression of E6 and E7 genes, and may also dysregulate oncogenes near the sites of viral insertion
In precancerous conditions like Condylomata viral DNA is present in episomal form (extrachromosomal form).
The most frequent types of cervical cancer are squamous-cell carcinoma and adenocarcinoma, which develop from the distinctive precursor lesions cervical intraepithelial neoplasia (CIN) / squamous intraepithelial lesion (SIL), and adenocarcinoma in situ (AIS), respectively. Their tumorigenesis is HPV-related. High-risk HPV (e.g., types 16 and 18) is integrated into the genome and leads to tumor progression. Cytological screening leads to detection of precursors and their mimics. P16 and Ki-67 immunohistochemistry assists in the histological differential diagnosis of precursors to reactive and metaplastic epithelium. For invasive cervical carcinoma, stage is the strongest prognostic factor. Per definition, microinvasive (pT1a1 / pT1a2) carcinoma is diagnosed histologically on cone biopsies and treated less radically. The distinction between adenocarcinomas of the cervix and endometrial adenocarcinomas is important and can be supported by immunohistochemistry (e.g., ER, p16, CEA, and vimentin) and HPV in-situ hybridization. The rarer adenoid-basal and neuroendocrine carcinomas are less frequently HPV-related.
Cervical Cancer Causes
Cervical cancer begins with unusual changes in your tissue. Most cases are linked to infection with human papillomavirus (HPV). Different types of HPV can cause skin warts, genital warts, and other skin disorders. Others are linked to cancers involving the vulva, vagina, penis, anus, tongue, and tonsils.
Cervical Cancer Risk Factors
You might be at higher risk of cervical cancer if you:
- Started having sex before age 16 or within a year of starting your period
- Have multiple sexual partners
- Take birth control pills, especially for longer than 5 years
- Smoke cigarettes
- Have a weakened immune system
- Have a sexually transmitted disease (STD)
Cervical Cancer Symptoms
You might not notice symptoms of cervical cancer until it’s far along. They may include:
- when you have sex
- Unusual vaginal bleeding, such as after sex, between periods, after menopause, or after a pelvic exam
- Unusual vaginal discharge
After it has spread, the cancer can cause:
- Pelvic pain
- Trouble peeing
- Swollen legs
- Kidney failure
- Bone pain
- Weight loss and lack of appetite
- Fatigue
Cervical Cancer Diagnosis and Exams
The most important advance in cervical cancer screening is broader use of the Papanicolaou test (Pap smear) and high-risk HPV testing. A Pap smear is part of a woman’s regular pelvic exam. Your doctor collects cells from the surface of your cervix, and a technician looks at them under a microscope. If they spot anything unusual, your doctor will take out a bit of cervical tissue in a procedure called a biopsy.
Other tools can find changes in your cervix. They include:
A colposcopy is a like a pelvic exam. Your doctor may use it if a Pap smear finds unusual cells. They stain your cervix with a harmless dye or acetic acid so the cells are easier to see. Then, they use a microscope called a colposcope, which magnifies your cervix by eight to 15 times, to look for unusual cells for biopsy. You can usually have this procedure in your gynecologist's office. You might need another biopsy later if the colposcopy shows signs of invasive cancer.
In the loop electrosurgical excision procedure (LEEP), your doctor uses an electrified loop of wire to take a sample of tissue from your cervix. You might have this in your gynecologist's office.
Your doctor can do a conization (removal of part of your cervix) in the operating room while you’re under anesthesia. They might use a LEEP, a scalpel (cold knife conization), or a laser. These are usually outpatient procedures, so you can go home the same day.
LEEP and cold knife conization procedures give your doctor a better look at the types of unusual cells in your cervix and whether they’ve spread.
Precancerous changes
Unusual changes in cells on the surface of your cervix are usually called squamous intraepithelial lesions (SIL). "Lesion" means an area of unusual tissue; “intraepithelial” means these cells are only in the surface layer.
These are precancerous cells. They might not become cancerous or invade deeper layers of tissue for months or years.
Invasive cancer
If a biopsy shows cancer that’s further along, your doctor will probably do more tests to see whether it’s spread and how far. They include:
- A chest X-ray to check your lungs
- Blood tests to see whether it’s spread to your liver; you might have a CT scan to refine the results
- An intravenous pyelogram (IVP) or CT scan to look at your urinary tract; a cystoscopy can check your bladder and urethra
- A colposcopy to look at your vagina
- A proctosigmoidoscopy and barium enema to check your rectum
- CT, MRI, or PET scans of your lymph nodes
- Treatment for Precancerous Lesions
If you have a low-grade lesion, you may not need treatment, especially if your doctor took out the area during a biopsy. Get regular checkups to watch for problems later on.
Your doctor might use LEEP conization, cold knife conization, cryosurgery (freezing), cauterization (burning, also called diathermy), or laser surgery to destroy the precancerous area with little damage to nearby healthy tissue.
In cryocautery, a steel tool that’s cooled to subzero temperatures freezes cells on the surface of your cervix. They die and fall off, to be replaced by new cells.
Laser ablation uses a laser beam to destroy cells in areas or layers of cervical tissue, leaving healthy cells in their place.
You’ll need a follow-up exam and Pap smear after cryocautery or laser ablation to make sure all the precancerous cells are gone.
You could also have a hysterectomy, in which your doctor removes your uterus. It will keep you from getting cervical cancer. But because it takes out your reproductive organs, you can’t become pregnant afterward.
Cervical Cancer Treatment
Surgery and radiation therapy are the most common treatments for invasive cervical cancer. Others are chemotherapy and biological therapy.
If the cancer is only on the surface of your cervix, your doctor can remove or destroy the cancerous cells with procedures like LEEP or cold knife conization.
If cancerous cells have passed through a layer called the basement membrane, which separates the surface of your cervix from underlying layers, you’ll probably need surgery. If the disease has invaded deeper layers of your cervix but hasn’t spread to other parts of your body, you might have an operation to take out the tumor.
If it’s spread into your uterus, your doctor will probably recommend a hysterectomy. Talk with them about the pros and cons.
Radiation therapy (or radiotherapy) uses high-energy rays to damage cancer cells and stop their growth. As with surgery, the radiation affects cancer cells only in the treated area.
Your treatments might be external, internal, or both.
External radiation comes from a large machine that aims a beam of radiation at your pelvis. You’ll probably get treatments, which take only a few minutes, 5 days a week for 5 to 6 weeks. Finally, you may have an extra dose of radiation called a "boost."
Internal radiation (also called implant radiation or brachytherapy) comes from a capsule containing radioactive material, which your doctor puts into your cervix. The implant puts cancer-killing rays close to the tumor while sparing most of the healthy tissue around it.
Chemotherapy uses powerful drugs to kill cancer cells. Doctors often use it for cervical cancer that’s locally advanced or has spread to other parts of the body.
Chemotherapy happens in cycles of intensive treatment followed by recovery periods. Most people have it as an outpatient (in an outpatient clinic at the hospital, at the doctor's office, or at home).
Biological therapy or immunotherapy targets “checkpoints” in your immune cells that are turned on or off to set off an immune response. A medicine called pembrolizumab (Keytruda) blocks a protein on the cells to shrink tumors or slow their growth.
Doctors use it if chemo isn’t working or if the cancer has spread. You’ll get it through a vein (called intravenous, or IV) every 3 weeks.
Outlook for Cervical Cancer
The survival rate is close to 100% when you find and treat precancerous or early cancerous changes. The prognosis for invasive cervical cancer depends on the stage.
- More than 90% of women with stage 0 survive at least 5 years after diagnosis.
- Stage I cervical cancer patients have a 5-year survival rate of 80% to 93%.
- Women with stage II cervical cancer have a 5-year survival rate of 58% to 63%.
- The survival rate for women with stage III cervical cancer is 32% to 35%.
- Sixteen percent or fewer women with stage IV cervical cancer survive 5 years.
Health care providers who treat cancer often use the term "remission" rather than "cure." Many women who have cervical cancer recover completely, but it can still come back



































Comments
Post a Comment